- Researchers at Amgen British Columbia are using human tonsil and 3D bioprinted tissue to mimic the immune system outside of the body.
- The immune tissue platforms have the potential to test whether a drug in development will provoke an immune response before it reaches the clinic.
- The platforms will generate data to drive machine learning algorithms that could predict immune responses in drugs in development more quickly and efficiently.
- The platforms may also assist in producing new antibodies for development.
One of the biggest pain points during drug development is predicting which protein-based medicines will prompt an immune response that may neutralize the molecule before it has a chance to do its job.
Finding better ways to test how the highly complex human immune system will respond to an investigational drug before it reaches the clinic has proven to be very difficult. Mouse models tend not to reflect human immunity well, and human immune cells from blood do not behave the same way that they normally do in the body.
"This is one of the big challenges we still have in drug development – not being able to predict what will happen in humans in terms of immune responses," said Chadwick King, executive director of Research and site head of Amgen British Columbia, Amgen's Canadian research site rooted in the study of antibody-based medicines. The site is celebrating its 20th anniversary this year.
A new use for tonsil tissue
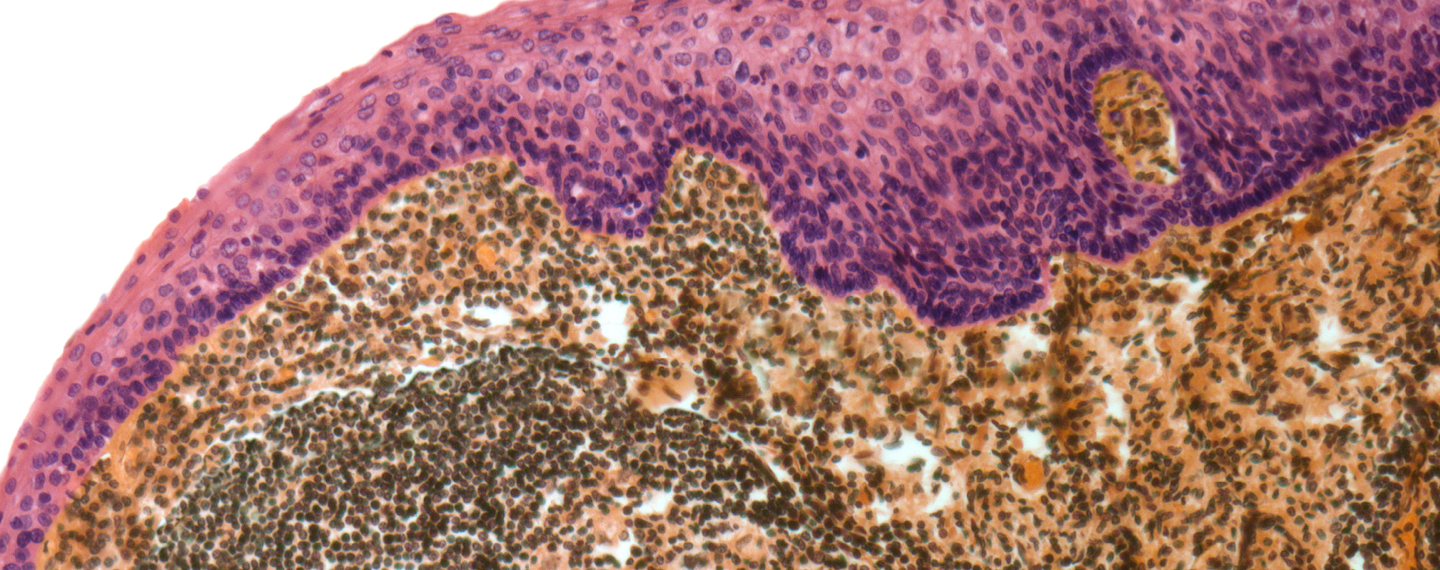
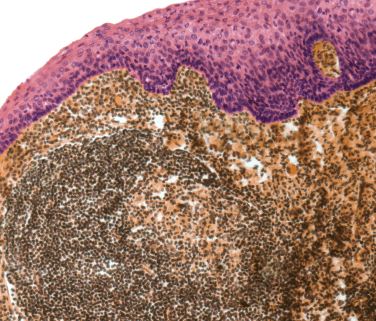
Researchers there are using human tonsil tissue obtained from tonsillectomies (when tonsil tissue is removed surgically) to create a complex cell culture platform that mimics the human immune response in tonsils but can grow and be studied outside of the body.
Tonsil tissue is one form of defense against infectious agents that enter the body when we breathe in or swallow. Located at the back of the throat, the tissue contains a rich source of immune cells, including B cells, that produce antibodies, and helper T cells that prompt B cells to make targeted antibodies. Lymph nodes are another example of an immune tissue that helps the body fight infection.
When the researchers provided the materials needed to grow, or culture, the tonsil tissue in the lab, the cells spontaneously formed 3D clusters that behave similarly to how they would in the body. The scientists plan to use these cultures to test medicines being developed to get a better idea of whether a drug will provoke an immune response.
"We are investing in assays that allow greater prediction of biology," said King. "In this case we are using three-dimensional organoid-like structures that allow us to better replicate human immunity. The long-term goal is to learn from this biology so we can better predict immunity using Artificial Intelligence (AI) and Machine Learning (ML) in the future."
Promising early results
The platform has already been tested against compounds known to provoke or evade immune responses. The cells behaved as expected in both cases. This shows that the platform can replicate whether or not there is an immune response to these known compounds.
"Until we started getting into these next generation tissue platforms, there was no way to generate accurate data about how the human immune system might respond to some of these drugs until they reached the clinic," said Mario Fidanza, the lead scientist at Amgen British Columbia working on the immune tissue platforms. "This data is going to be really valuable going forward."
The research team plans to expand its tonsil organoid platform by creating an in-house biobank of tonsil tissue, said King. This will allow them to study a broader population to identify and better understand a wide variety of immune responses to the drugs Amgen develops.
This immune tissue work is being done in close collaboration with Amgen colleagues in the clinical immunology group, who assess risk of immune responses to medicines in development using conventional platforms. These standard platforms are generally not able to predict why immune responses to certain drugs occur once they reach the clinic.
Predicting immune responses in screening assays such as this tissue platform (in the wet lab) or from the molecule's sequence (computationally) will allow researchers to decrease the chance that a clinical trial will fail because a drug has triggered an immune response.
Building model immune tissues from scratch for antibody discovery
The team is also collaborating with FluidForm, a company that specializes in human tissue bioprinting technology. The researchers are working on combining cells and engineered molecules as building blocks needed to make immune tissue. They then plan to use FluidForm's FRESH™ platform to 3D bioprint the tissue. Building tissues from scratch creates the opportunity to customize or engineer all the components necessary to have greater control over various types of immune responses.
The human immune system becomes "educated" to tolerate certain molecules, or antigens, such as ones produced by the body's own cells. This can protect the body from attacking itself and developing autoimmune diseases. But it can be a problem when making human antibody drugs that seek to target molecules similar to ones that the immune system has become tolerant to.
Tonsil tissue may not produce useful antibodies to a target of interest that the immune system has learned to tolerate. But an engineered immune tissue platform made from scratch would not yet have that education and might have the potential to be coaxed into producing antibodies to a disease target, even if it looks similar to a normally tolerated human antigen. The new platform may also potentially help with the discovery of human antibodies that could form the bases for new medicines.
Bioprinted tissues offer many advantages, said Fidanza. They reduce the dependance on precious human-derived samples and may prove to be more scalable and able to answer more specific research questions about the immune system as these models are applied more broadly across the discovery and development process.
Learn more about Amgen's human antibody discovery platform.